Miguel is not going to let anything get in the way of telling his story. Of the three people we talk to on this sunny morning at the HIV facility where he lives in Cartago, he is the first to volunteer to tell his story; he is the only one who is willing to publish his real name and image; and he is the oldest, at 46. He says that his age is a big part of his current attitude. He doesn’t have any time to waste.
“I’m practically a senior citizen,” he says with the mirth that runs throughout his narrative, hard though his life has been—but his comments about his future are all about getting serious. He wants to finish a university degree in psychology. He wants to invest his time in a relationship with his adult son. He wants to make permanent the changes he has implemented during his time at the Nuestra Señora de la Esperanza HIV Home: leaving behind the addiction to drugs that led to his years living on the streets of San José, and time in various prisons.

That’s another possible reason for Miguel’s open approach, as well as his quickness to bring up HIV discrimination as the biggest challenge facing people as the virus in Costa Rica: as a gay man who has lived in the streets and experienced years of addiction, he has experienced some of Costa Rica’s worst stigmas three times over. He explains that the stigma attached to the virus and the misinformation he received had a direct and negative impact on his mental state and, therefore, on his adherence to treatment. He says that because he thought that HIV was a quick death sentence, he ignored his treatment options, until he eventually made his way to the Hogar Nuestra Señora de la Esperanza and learned for the first time how the virus actually works and can be controlled.
“I was diagnosed with HIV in 2011, and I wanted to die fast,” he says. “I had a lot of prejudices and lots of bad information about HIV, so I thought that since I was eating out of the garbage and sleeping on cardboard boxes, AIDS would be a quick death—and that’s just what I wanted… I was disgusted by my own body. If I got cut, I was disgusted by my own blood. I was disgusted by my own saliva. I didn’t want to touch anyone, or hug my kid, or shake his hand.”
He says the stigma around the virus was the worst part of the diagnosis.
“It was a huge shock,” he says. “I don’t think it was the news itself. It was more about my prejudices about it, all the stigma that goes with VIH. For gay people, it’s a punishment from God, and you can’t kiss anymore. You can’t share anything.”
This led him to start, then stop, his HIV treatment multiple times, until a few twists of fate led him to take his treatment more seriously. The first was falling ill with tuberculosis.
“I was hospitalized,” he says. “It was a painful, bitter experience. It’s easy to say ‘I want to get sick and die,’ but once I was in the hospital I realized how much suffering there was, everything you have to go through when you’re there. I had to spend half an hour just thinking about going to the bathroom [before I could get up]. I got scared, and I said, ‘No. I don’t think so. I don’t want to get AIDS and die like this.’”
Another twist of fate was a chance encounter in the hallway of a clinic with a former partner who worked there as a doctor was helpful to Miguel: the doctor took him aside and explained that he could live a long life with the virus, something he hadn’t understood beforehand.
If it hadn’t been for that conversation, Miguel says, he would have lacked that basic understanding—much like his two housemates at Nuestra Señora, Sofía* and Alonso*, who are sitting at the table with him. Alonso even says that when he was first diagnosed, he was actually told he had AIDS rather than HIV. Full of pessimism, all three of these HIV-positive interviewees failed to take their medication, thinking that they were doomed anyway.
While, as reported in Part II, Costa Rica’s interdisciplinary HIV clinics are a valuable source of quality information for people with the virus, Sofía and her housemates point to the stigma and discrimination they’ve faced when dealing with health staff outside of the clinics, and the general public.
“I’m surprised that there are so many people in the Calderón Guardia itself, or who are working in the [regional and local] health areas,” without correct information, Sofía says. “How are they not going to be informed? And how do they not know the difference between HIV and AIDS?”
Health care providers who specialize in HIV reinforce these stories—such as psychologists Noelia Solano and Nelson Chacón, who together lead the mental health care support for Nuestra Señora’s residents. Noelia says that anecdotes such as Alonso’s are common.

“Just last week a [resident] told me that in an appointment he had recently… the doctor said to him, ‘Right, so I’m just going to note here that you have AIDS’,” says Noelia. “He comes back here and says to me, ‘I don’t have AIDS, do I?” I said to him, “Was it the doctor who said that to you?” He said, “Yes, it was the doctor.” I find it incredible that the doctor himself… would make a mistake like that.”
With errors like this at the level of medical professionals, it goes without saying that misconceptions about HIV are widespread among family members with the virus, Nelson says.
“The impact of social disinformation about people living with HIV is extremely complex, because it begins with our families,” he says, echoing Miguel’s words about not being able to hold his nephew, or Sophia’s story about her separate plate. “There’s labeling, rejection and discrimination in our very first institution, which is our family. That’s where the tragedy begins for many of these people, because they’re thrown out of their homes; their support networks cease to exist; and oftentimes, these people, thanks to that family rejection, make incorrect decisions, such as substance abuse, prostitution, or living on the street. There’s a huge loss of self-confidence and self-esteem.”
Dr. David Reyna—a specialist in palliative care and HIV, and a part of the team at the HIV clinic at the Hospital México—echoes this statement.
“The lack of general knowledge in the population [about HIV] is massive, and unfortunately this includes some health staff,” he says. “You still find comments of patients who go to the dentist and they put off their appointments, or they go to a surgeon and the surgeon refuses to operate on them. It’s striking how at this point, right in the 21st century, we’re still facing such widespread ignorance. And this affects the person’s self-esteem and has a direct impact on their acceptance of their diagnosis and their adherence to treatment.”
So what’s the opinion of public health authorities about this issue, and what’s being done to address it?
José Pablo Montoya and Maricruz Pérez of the Ministry of Public Health spoke to me via Zoom about these challenges. According to José Pablo, a representative of the National Council on Integral Attention for HIV-AIDS (CONASIDA), one factor that might explain some of the reports of misinformed health staff might have stemmed from an advance. He explains that to address the need to decentralize HIV services that Dr. David Reyna mentions above, in 2018, HIV testing processes were decentralized so that community health teams, or EBAIS, can perform a test and then refer patients up the ladder to an HIV clinic. This vastly increases access to HIV testing, but means that the person giving you the result “might be a general doctor or a nurse who might not have breadth or depth of criteria about HIV, the way they do in the HIV clinics.
“Not that we’ve never had a situation like that in the clinics themselves,” he adds, referring to the overall saturation of Costa Rica’s public health facilities. Even at one of the HIV clinics, he says, you might have a doctor who is fully informed about HIV but has only the regulation 15 minutes to do various things with a new patient.
“It’s a complex infection,” he says. “When it comes to adherence, you have to explain to patients about all the care they need to take with their medication. With nutrition. Sleeping well, having healthy habits, avoid drug use, taking the pill at the right time… and then there’s mental health. If a person has better mental health, they’ll have better adherence. So imagine yourself having to explain all those things in 15 minutes… You think, ‘Good lord!’”

The new EDUS digital file system requires that doctors input patient information into digital files, reducing the time still further; and many health centers have seen the 15-minute mark recede into the background, with only 7 or 8 minutes per patient.
Putting the problem of over-saturation aside, the Health Ministry is currently training regional health staff to address the information gap and address HIV stigma. Over recent years, inter-institutional HIV networks have been created in various areas outside the Central Valley—starting with San Carlos, Limón, and Puntarenas, before expanding to include the Huetar Norte—and this year, to support this process, the ministry is training approximately 200 officials in its regional and local departments. Maricruz Leiva explains that the trainings have included information about current status of the HIV epidemic in Costa Rica and medical advances, as well as “healthy and holistic sexuality, stigma, and discrimination, with a focus on and diversity.” The results of the training will be evaluated in January 2024 before moving on to include more personnel.
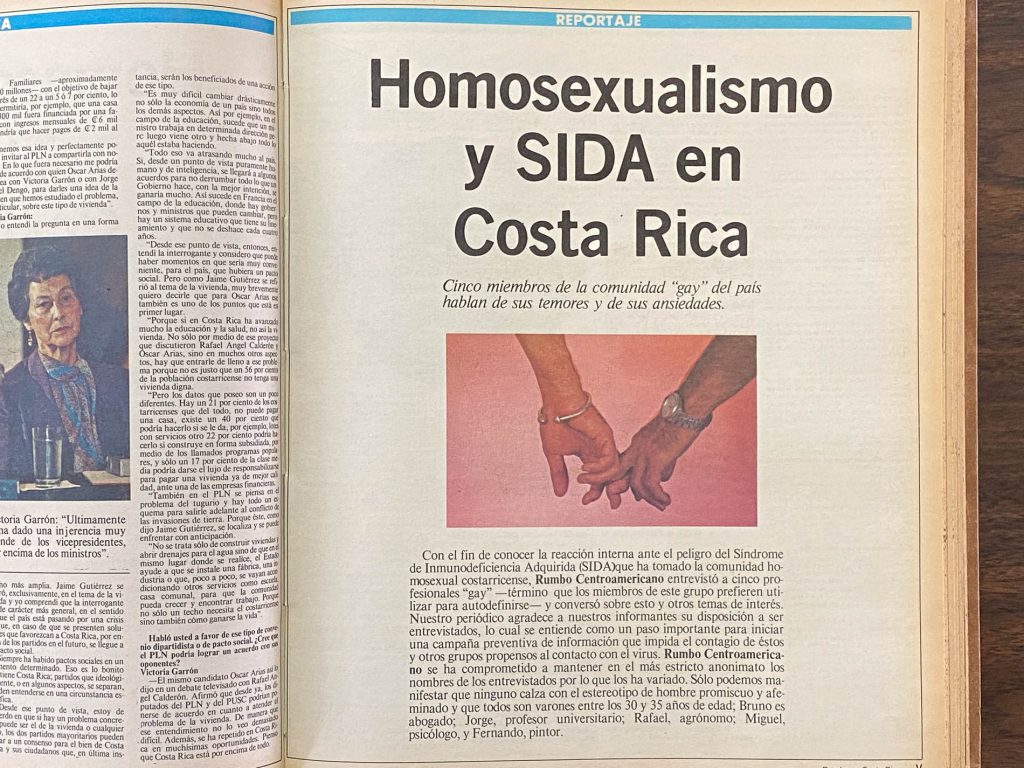
“In our culture, which includes health personnel… there are myths, erroneous beliefs,” José Pablo says. “Maybe no one ever explained to them the basics of sexually transmitted diseases, or they still have this idea of HIV-AIDS from the 80s and 90s: that it’s a death sentence. The goal of these [trainings] has been to knock down those closed conceptions.”
What’s clear from discussions with Miguel, however, is that efforts like these to chip away at misconceptions, while important, will simply not be fast enough. Especially not for Miguel, who has a clear sense of time slipping away.
“I used to say, ‘I have so much time ahead of me. I’m so young, I’ve got the whole world in my hands,’” he says. “Not anymore. I’m getting older. Ya soy un señor. It has to be now.”

People grappling with a foe like HIV and the mental health challenges it brings along with it—especially when combined with addiction—need intensive support and lots of resources. They need to be surrounded by well-informed professionals, not just occasionally, but throughout their day-to-day-life, say Nelson and Noelia. And they need this right away.
When they get that level of attention, the results can be jaw-dropping. Next time: Alonso shows us why.
This longform piece, published in four parts, was supported by the Internews Health Journalism Network. Learn more about the Nuestra Señora de la Esperanza HIV Home on their Facebook page or donate via SINPE Móvil at 8507-7676. Learn more about Dr. David Reyna’s Care with Love Foundation here.
*The real names of Sofía and Alonso have been withheld at their request, to protect their privacy and in consideration of the discrimination that is faced by people with HIV in Costa Rica.